COVID-19 INFECTION FATALITY RATE SIMILAR TO A BAD FLU
In summary….
- Many more people have become infected (IFR) than come to medical attention, become a case, and succumb to COVID-19 illness (CFR)
- Infection fatality rate from an updated, comprehensive review of available studies is now closer to 0.15%, similar to a bad flu season, or at worst a prior flu pandemic
- While COVID-19 death statistics appear subject to manipulation and overcounting, most appear in those with severe underlying health conditions, often near the end of normal life expectancy
- “Long-haul COVID” symptoms are concerning although not unique to COVID-19 and may also occur following COVID vaccination
Claim 12: Blood testing shows many more people have been infected with COVID-19 than official statistics, meaning it’s not much more lethal than the flu
NH COUNTERCLAIM: The case fatality rate (CFR) for COVID-19 to date is 2.1 percent – that is 2.1 percent of all known cases have resulted in death. Though both the number of dead and number infected are believed to be undercounts, it’s likely far more infections than deaths have been missed thanks to a lack of testing, particularly in poorer countries and in the pandemic’s early months.
DrPC: The distinction between infection fatality rate (IFR) and case fatality rate (CFR) is important, as they differ greatly, and will be explained below.
The IFR counts deaths by comparing a projected number of individuals in a population, country by country, region by region, who have evidence that their bodies have “seen” the virus and that their immune systems have become activated in one of several ways to respond to the viral incursion (by SARS-CoV-2 in this case) in defence.
By convention, however, only the antibody levels to the virus are considered, and these may taper after several months after exposure to the virus, and thus may contribute to overestimating IFR. Cellular immunity, while important and demonstrated in research studies, is not considered, and thus this method will also under-count those who have been infected with SARS-CoV-2.
Importantly, deaths along with COVID-19 are often counted the same as deaths from COVID-19, causing major issues with accuracy of both IFR and CFR, and we will come back to that later.
The projected number of individuals that have been exposed to the virus is estimated by taking a small and ideally representative sample of the overall population, and applying the percentage infected to the whole number of the entire population.
Since there is a far greater number of individuals who have been infected but had no symptoms, or had symptoms so mild that they never sought medical attention or got tested, the IFR will, as expected, be much lower than the CFR.
Many more people are infected (IFR) than come to medical attention, become a case, and succumb to COVID-19 (CFR)
NH: [continuing…] This means the infection fatality rate (IFR) is likely to be lower than 2.1 percent, but just how much lower isn’t known. The best estimates to date range between 0.5 percent (about five times more lethal than influenza) and 1.5 percent, though it’s much higher for the elderly and lower for children.
Seroprevalence testing looks for the presence of antibodies to the disease. Dr Canaday says research hosted on the World Health Organization’s own site suggests it could be as low as 0.2 percent, making it only twice as lethal as the flu. That study was carried out by John Ioannidis, whose other papers on the lethality of COVID-19 have been heavily criticised by other epidemiologists.
Imperial College London estimates the IFR to be between 0.14 percent and 1.79 percent, depending on the makeup of a local population. Its research says figuring out the true figure is “challenging due to the dynamic and imperfect nature of the available data”, but it’s “substantially higher than IFR estimates for seasonal influenza.”
DrPC: Background fatality rates (IFR) for influenza vary from year to year by age, country, and demographics, estimated at 0.1% to 0.5% in a recent paper. (R1) There was wide variability in estimated fatality rate from the 2009 H1N1 pandemic flu, from 0.01% to 13% depending on whether the comparison was from evidence of infection from serologic studies, or based on symptoms, or based on laboratory confirmed specific culture of influenza virus and thus not an “influenza-like illness” known as ILI. (R1A)
However, since the COVID-19 pandemic began in earnest in March 2020, hospitalisations in the US for lab-proven influenza and respiratory syncytial virus (RSV) fell dramatically, by 99% (R2) with deaths expected to follow a similar trajectory. This likely represents a “displacement” process whereby respiratory illnesses usually caused by influenza were displaced by the more infectious and purportedly “novel” coronavirus, as has happened before. (R3) See also response #13.
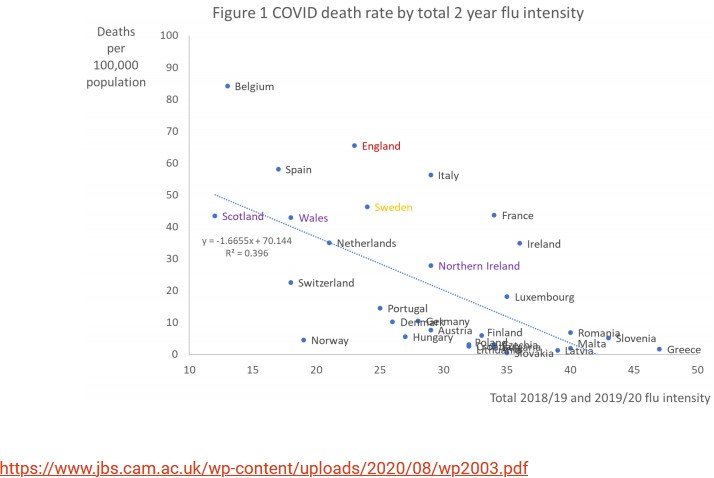
In truth, somewhere between 20,000 to 45,000 of the “usual” annual influenza deaths in the USA may well have been replaced by “COVID-19” deaths since the pandemic began. This “displacement” effect of COVID-19 was more apparent in countries which had previously mild influenza seasons: (R3A, R3B)
Of note, an update to Dr Ioannidis’s original paper from 2020 was published in 2021, based on a review of seroprevalence data from several globally canvassed studies. These data indicate that the true IFR is likely 0.15% overall, which is lower than his original 2020 estimate of 0.23% (R4). Furthermore, it is closer to 0.05% for those under 70, which is actually similar to that for influenza. (R5) The recent Ioannidis paper evaluated 1085 publicly available titles and selected six with sufficiently rigourous methodology for inclusion. Studies lacking robust scientific methodology were considered unsuitable for inclusion in his review and may well have been responsible for the “best estimates” alleged by the NewsHub source.
As far as Imperial College London is concerned, only a few months into the pandemic, Neil Ferguson’s estimates of expected mortality were known to have wildly overestimated deaths from COVID-19, by a factor of at least 10. (R6) His work has often been well off the mark in the past, and come under criticism for wild inaccuracies. (R6A)
Infection fatality rate from an updated, comprehensive review of available studies is now closer to 0.15% and similar to a bad flu season
NH: The IFR can also be heavily dependent on the demographic makeup of a population, and how sturdy its health system is – if hospitals get overloaded, more people will die that would have otherwise lived if they had access to timely treatment. Australian doctors have warned this might happen if the country opens up too soon.
DrPC: Indeed, the IFR depends on a number of factors, including demographic makeup, the integrity of the testing and reporting systems for COVID-19, and the sturdiness of the health care systems, and each of these parameters was among the factors considered in Dr Ioannidis’s review. Nevertheless, we can see how even the raw COVID-19 mortality rate differs greatly among various countries as a result, (although for a moment we will digress to what amounts to a CASE FATALITY RATE):
Despite the inherent variability in age and demographics of each country, the global average IFR was calculated to be 0.15%. Granted, the paper retrieved reliable data primarily from Europe and North America, and likely missed other countries with younger populations, those with fewer care home residents, and thus did not include studies from countries with an inherently lower IFR. (Notably, the Ioannidis study was largely based on reports published early to mid-way through the pandemic; studies were not yet been available from those other countries.)
An insightful post published in September 2020 suggested that the Director of the National Institute of Allergy and Infectious Disease, Dr Anthony Fauci, had meant to assign an IFR of 1% to COVID-19 and 0.1% for influenza, where a CFR for COVID-19 at 2-3% had been similar to that for H1N1 “swine” flu in 2009. (R6B) The author states that later estimates of COVID-19 IFR from the WHO and CDC had fallen to 0.65%, and now we have estimates from Ioannidis’s paper that have fallen further still from 0.23% in his original study from September 2020, and finally to 0.15% in his January 2021 paper on “reconciliation”.
It appears that as time went on, the calculated IFR for COVID-19 fell further and further until it did indeed approach that of influenza.
All studies, of course, confirmed that IFR was much higher in the older populations, especially in the care homes. It is important to note, when considering the lethality of COVID-19, however, is the author’s reference demonstrating that even “common cold” coronaviruses have a case fatality rate (CFR) of 10% in care home outbreaks, where 20% of deaths occurred even in those without co-morbidities. (R7)
As for criticism of Dr Ioannidis, previously a highly respected, and globally prominent epidemiologist until his inconvenient publications, I don’t think we should put too much faith in a journalist-acquaintance writing for a left-wing general audience publication, where criticism was propelled by the author’s conclusions that lockdowns and the expected social and economic disruptions should perhaps be questioned. (R8)
NH: He [Ioannidis] once predicted just 10,000 Americans would die of COVID-19 before it was over – so far, more than 600,000 have died. About 10,000 have lost their lives in the past week alone.
DrPC: So, here’s the problem with mortality counts. Seroprevalence studies used to determine how many people have been exposed to the virus are denoted by the denominator of the fractional IFR. Although that’s primarily what Dr Ioannidis’s paper addressed (because underestimating the number infected will inflate the IFR), the numerator matters, too. That’s the estimated number of deaths in each country represented in the analysis, and attributing deaths to COVID-19 has proven to be problematic.
For the numerator of the IFR, but especially for the numerator in the CFR, one must be careful about overestimating total deaths due to COVID-19. The CFR counts deaths where an individual has come to medical attention (or at least has come to a PCR testing station initially based on self-described symptoms) and has then been treated unsuccessfully, perhaps first as an outpatient, then hospitalised, and has then failed all attempts at treatment.
However, deaths attributed to COVID-19 may all be considered as one or more of the following:
- Positive PCR test and symptoms due to a flu-like illness with characteristics that appear unique to COVID-19, such as systemic inflammatory syndrome, cytokine storm, perhaps with or without stroke, heart attack or signs of thromboembolism,
- Positive PCR test with typical flu-like illness as above, but actually due to coexisting influenza or another respiratory virus where the PCR test was a false positive (see my NewsHub response #3)
- Suspected COVID-19 in the absence of a positive PCR test but where clinical presentation and course were “believed” to be due to COVID-19, or where a positive PCR test was obtained after admission to hospital where in hospital viral transmission may have occurred
- Deaths due to unrelated causes where a positive PCR test was obtained within 28 days of death, which may account for a large and substantial number of overcounts. More on this later.
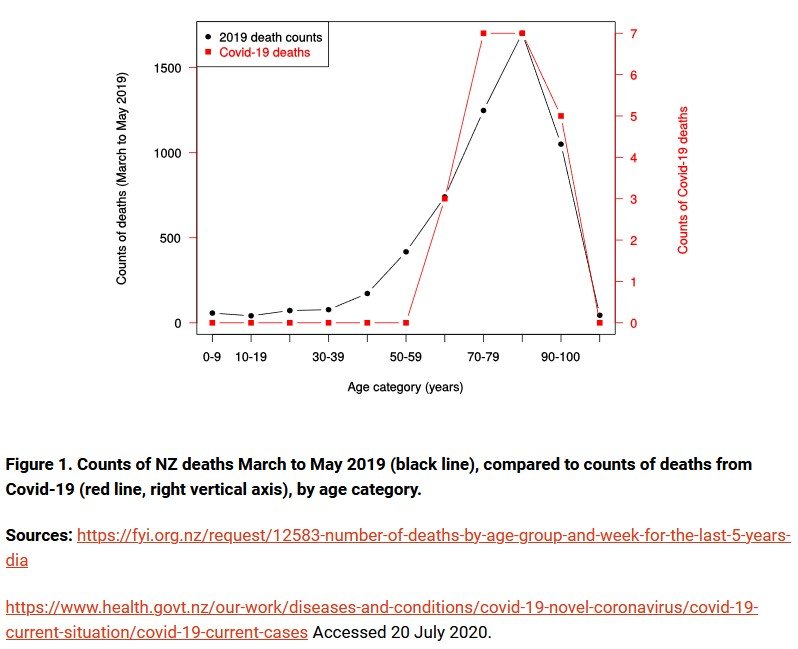
It is also known that, at least in the main course of the pandemic, average age of death from COVID-19 was very close to the natural life expectancy, as in NZ: (R9)
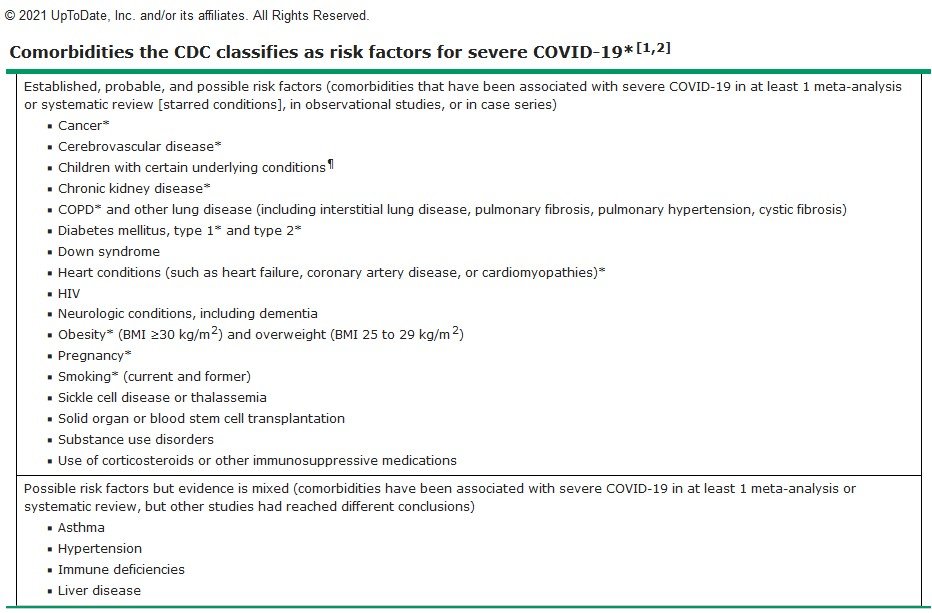
However, more to the point is that many deaths recorded as due to COVID-19 were in those with significant underlying “co-morbid” conditions, in other words, diseases that made them more vulnerable to succumbing to a viral respiratory illness, indeed, ANY viral respiratory illness. Underlying conditions such as heart and respiratory disease (viz chronic bronchitis, asthma, and emphysema), high blood pressure, diabetes, stroke, dementia, and cancer made up a large proportion of these conditions. (R10) Indeed, only 6% of deaths due to COVID-19 were not accompanied by some other condition, according to CDC records in the USA. (R11)
Nevertheless, at the beginning of the pandemic, COVID-19 was elevated to the main cause of death on death certificates instead of a “contributing” cause of death. Shockingly, sometimes COVID-19 was even listed in state and federal level statistics in the USA where a PCR test had been positive within 28 days of death although COVID-19 was never diagnosed clinically, as in murders, suicides, motor vehicle accidents or cancer. On some occasions, a COVID-19 death was recorded even in the presence of a negative PCR test! (R12, R13) Further, the director of the CDC, Dr Robert Redfield, has had to acknowledge that the counts have been inflated. (R14)
While COVID-19 death statistics appear subject to manipulation and over-counting, most appear in those with severe underlying health conditions, often near the end of normal life expectancy
NH: Dr Campbell said there have been a “lot of papers” in this area with varying results, and focusing on just the IFR ignores the long-term suffering many survivors will experience, including neurological and cardiovascular damage, not to mention long COVID.
DrPC: Yes, there can be long-term consequences of COVID-19 illness, as indeed there can be and have been negative long-term consequences following COVID-19 vaccinations. The prevalence and nature of these conditions is difficult to compare, although the FDA, in a confidential briefing on 22/10/2020, acknowledged in their draft working list of possible adverse outcomes following COVID-19 vaccinations the following:
Many of the adverse effects, including neurologic and cardiovascular effects that are associated with COVID-19 disease as noted above, have also been associated with the COVID-19 vaccines. This should not come entirely as a surprise, since the toxic effects of the SARS-Co-V2 virus have been traced to the spike protein, which in altered form is the very basis of COVID-19 vaccination (both mRNA and DNA vector types). (R15, R16) For perspective, it is also important to remember that “long-haul COVID” symptoms are not unique to SARS-CoV-2 viral infection but have been seen historically following other viral illnesses for quite some time. (R17)
“Long-haul COVID” symptoms are concerning although not unique to COVID-19 and may occur also following COVID vaccination
SUMMARY AND IMPLICATIONS
We must try to distinguish the case fatality rate (CFR), where deaths are counted among those with a positive PCR test, from infection fatality rate (IFR), where the deaths are compared to the much larger number of those who have evidence that their immune system has seen the COVID-19 virus, SARS-CoV-2, or in other words, all those that were infected.
When we do consider the IFR, we can confirm through a sturdy review of the available literature by Dr Ioannidis, that the risk of dying from COVID-19 is about 0.15% overall, and significantly lower if one is less than 70 years of age (but greater than that in those with other serious medical conditions).
It is important to remember that is the risk if you become infected, but many infections occur with few or no symptoms. Furthermore, not everyone will actually become infected either (although with the Delta variant it appears more likely one will be infected than during the initial wave of the pandemic). Nevertheless, the risk to the general population will likely be some degree lower than the general 0.15% IFR as well.
The COVID-19 pandemic has played the role usually reserved for the influenza virus in most winter seasons: carrying off those weakened by chronic health conditions. In the past, this has occurred even with the common cold coronaviruses. Still, at least until the prevalence of Delta and highly vaccinated populations, most deaths occurred in those close to their natural life expectancy. It remains to be seen whether that will now change.
As for counting COVID-19 deaths, there is legitimate concern and circumstantial evidence that these may be over-reported; the extent to which this has occurred is uncertain.
Without accurate data, and now with the determination that all those who’ve received their first jab, and even up to 14 days after their second shot, are considered “unvaccinated”, true death counts for COVID-19 may be further compromised.
Also, “long-haul COVID” is not unique to the SARS-CoV-2 virus or to COVID-19, but similar conditions have been seen following other viral illnesses.
The most important lesson in all this however is the following: infection fatality rates (IFR) and case fatality rates (CFR) depend on the number of fatalities. As time passed, better data were available about prevalence of those infected but not symptomatic, and treatment regimens also improved patients’ likelihood of survival. Both of these factors reduced IFR and CFR.
Imagine what would further happen to IFR and CFR if known effective and safe, repurposed drugs such as hydroxychloroquine and ivermectin were used more widely! These therapeutic alternatives are discussed elsewhere, including in response #24.
For further reading, consider CovidPlanB and Swiss Policy Research.
References:
R1: IFR for influenza. https://www.cdc.gov/flu/about/burden/past-seasons.html
R1A: Case fatality risk of influenza A (H1N1) from 2009. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3809029/
R2: What Effects have COVID had on respiratory virus patterns? https://www.medscape.org/viewarticle/959066?src=WNL_cmemp_211001_mscpedu_imed&impID=3680601&faf=1
R3: Why the flu has “disappeared.’ https://swprs.org/why-the-flu-has-disappeared/
R3A: From www.covidplanb.co.nz/category/data-science/page/6/ and https://www.jbs.cam.ac.uk/wp-content/uploads/2020/08/wp2003.pdf
R4: Reconciling estimates of global spread and IFR: An overview. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8250317/
R5: Covid-19 elimination debate needs correct data. https://www.bmj.com/content/371/bmj.m3883/rr
R6: Failed Imperial College models. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7301657/
R6A: Neil Ferguson and past inaccurate predictions. https://statmodeling.stat.columbia.edu/2020/05/08/so-the-real-scandal-is-why-did-anyone-ever-listen-to-this-guy/
R6B: Clarifying the true fatality rate, same as flu. https://medium.com/microbial-instincts/clarifying-the-true-fatality-rate-of-covid-19-same-as-the-flu-8148e38b9ab5
R7: Fatalities from common cold viruses in care homes. https://pubmed.ncbi.nlm.nih.gov/32720706/
R8: https://www.wired.com/story/prophet-of-scientific-rigor-and-a-covid-contrarian/
R9: From www.covidplanb.co.nz/category/data-science/page/7/
R10: Risk conditions for COVID-19. https://www.uptodate.com/contents/image?imageKey=PC%2F127477
R11: CDC confirms 6% of deaths associated with COVID-19 alone. https://www.cdc.gov/nchs/data/health_policy/covid19-comorbidity-expanded-12092020-508.pdf
R12: Sharyl Attkisson: Counting COVID | Full Measure. https://www.youtube.com/watch?v=DKwQlkKJ6Uo
R13: Inflated COVID death toll. https://www.realclearpolitics.com/articles/2020/05/29/us_covid-19_death_toll_is_inflated.html
R14: CDC director admits that COVID death counts are inflated. https://www.cnsnews.com/article/washington/melanie-arter/cdc-director-i-think-youre-correct-about-inflated-covid-death
R15: Spike protein accounts for tissue damage by itself. https://www.salk.edu/news-release/the-novel-coronavirus-spike-protein-plays-additional-key-role-in-illness/
R16: Spike protein damages blood vessels. Y Lei et al. Circulation Research. 2021;128:1323–1326. https://doi.org/10.1161/CIRCRESAHA.121.318902
R17: Long COVID not as unique as we thought. https://www.vox.com/22298751/long-term-side-effects-covid-19-hauler-symptoms. Contains references to medical sources.
CovidPlanB: https://www.covidplanb.co.nz/
Swiss Policy Research: https://swprs.org/covid-19-mortality-overview/